What is Dialectical Behavior Therapy (DBT)
Dialectical behavior therapy (DBT) is a research-based, cognitive behavioral therapy (CBT) developed in the late 70s by Marsha M. Linehan at the University of Washington. It was originally created for clients with suicidal thoughts and/or self-harm tendencies (often seen in clients with borderline personality disorder). Since DBT’s emergence in the 80s, it has expanded and is now used for clients with a wide range of struggles, issues, and diagnoses (eating disorders, post-traumatic stress disorder, substance abuse, etc.).
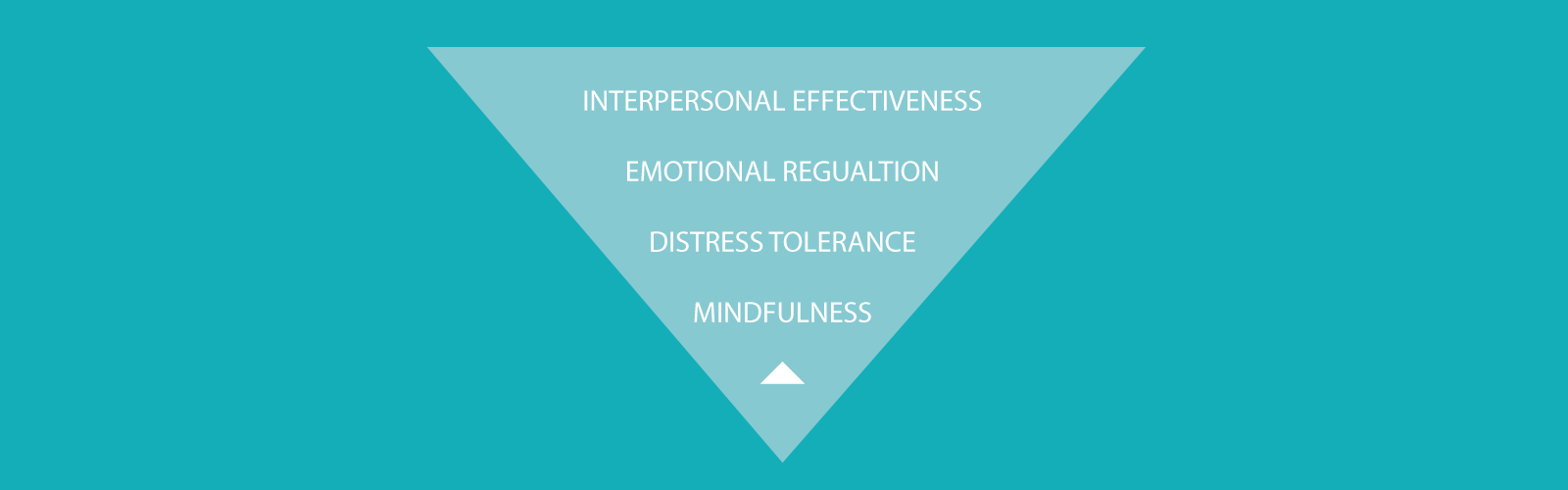
The Four Modules
Dialectical behavior therapy combines western and eastern contemplative practices and focuses on four areas (or modules):
- Mindfulness
- Distress tolerance
- Emotion regulation
- Interpersonal effectiveness
Mindfulness
Mindfulness skills taught in DBT surround paying attention to the present moment, both internally (emotionally) and externally. It is about experiencing one’s thoughts, feelings, and sensations fully, yet without judgment. Mindfulness is considered the foundation for the other skills taught in DBT.
Distress Tolerance
Distress tolerance emphasizes skills that help in accepting, finding meaning for, and tolerating distress and difficult emotions. Distress tolerance skills help individuals make healthy decisions, rather than acting/reacting out of emotional activation.
Emotion Regulation
The emotion regulation module in DBT focuses on skills that aid in regulating difficult emotions and decreasing the frequency and intensity of those emotions. Emotion regulation skills assist individuals in increasing awareness of emotions, reducing vulnerability to those emotions, and having an overall better understanding of how emotions affect them.
Interpersonal Effectiveness
Interpersonal effectiveness skills taught in DBT are similar to those taught in interpersonal problem-solving and assertiveness classes. Interpersonal effectiveness focuses on skills to ask for what one needs, and to say “no” (set a boundary.
Overall, DBT is designed to provide people with a more positive avenue of coping with emotions and challenging situations by changing unhelpful or unhealthy behavior patterns (such as substance abuse, gambling, suicidal thoughts, or tendencies toward self-harm).
The approach works by working with someone with these behaviors to improve emotional and/or cognitive regulation to better identify triggers that cause these behaviors. After the triggers are identified, a therapist will work with the patient to sort through the events, thoughts, and feelings that these triggers create in order to find healthier ways to channel them rather than repeating the same undesired behaviors. Dialectical behavior therapy operates under the assumption that most of us have flaws which we are trying to correct but are often lacking in certain skills or are easily influenced by positive or negative reinforcement which often interrupts our normal thought patterns or actions to bring forth undesirable behavior.
DBT & Psychotherapy
DBT can be used in a variety of mental health settings, with a variety of struggles or issues. Nonetheless, dialectical behavior therapy typically includes five components:
- Capability enhancement – this is where the development of coping skills and tools occurs. Here, clients are learning the skills (or enhancing their capability to use the skills), which are broken down by modules – mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Generalization – DBT therapists employ various techniques to encourage the skills to be incorporated by clients in numerous settings or areas of life – school, home, work, relationships, etc.
- Motivational enhancement – tracking records and self-monitoring logs are often used in DBT. These monitoring tools are meant to help clients identify unhelpful behaviors and unhealthy habits that may be affecting the overall quality of life. The records and logs can also increase client awareness to any patterns of behavior (i.e. – if a specific unhelpful behavior occurs more at night, at school, etc.)
- Capability and motivational enhancement of the therapist – DBT therapists receive supervision and support to prevent burnout, as DBT therapists often work with clients who suffer from severe mental illness.
- Structuring the environment – if a client participates in multiple treatment programs or has various providers (dialectical behavior therapy is often used in conjunction with other psychotherapy treatments), the DBT therapist will likely encourage all programs/providers to reinforce the use of the skills and behaviors taught in DBT.
DBT and Individual or Group Therapy
Research has shown DBT to be most effective when it includes weekly individual therapy coupled with a weekly skills-based therapy group. Thus, all dialectical behavior therapy should involve both components.
The individual sessions are one-on-one sessions with a therapist or counselor and client. Every individual session may look different, but in general, they tend to build upon the last session. Individual sessions are where the client can process current struggles and issues, learn skills and tools (and areas to apply those skills and tools), as well as reflect upon things that could have been done differently.
Dialectical behavior group therapy consists of a group of peers who may have similar struggles or mental health disorders. The groups are led by therapists or counselors specifically trained in DBT. Not only are skills and tools taught (from all four modules of DBT), but also how group members are using them and/or struggling to use them. DBT group therapy is also a means of support for those involved, as having others who struggle in similar ways and can personally relate can be a great source of comfort.
Through the four modules of DBT, clients are able to gain an increased sense of peace and participation in life, be more resilient, and strengthen interpersonal relationships. DBT can help clients gain a better understanding of themselves, their emotions, their triggers, and their self-sabotaging thoughts/feelings/ beliefs/habits.
Through ongoing practice and use of the skills taught in dialectical behavior therapy, clients may find they react to certain environmental, emotional, or interpersonal stimuli in a different, healthier way.
While none of the modules are as effective on their own, when used in conjunction with one another, and taught by a trained therapist (and a willing client), DBT can be hugely effective in helping clients improve their lives.
Post-Pandemic Update
During the COVID-19 pandemic, most of us experienced some level of anxiety, fear, or general sense of unease. As a result, we had to find ways to manage these emotions. Many turned towards things like food, alcohol, or drugs. In fact, studies show alcohol use rose by over 15%, unhealthy food intake rose by 25%, and smoking/vaping by almost 10%. And while these approaches may have felt effective in the moment, they likely created more problems in the long-run. Reflecting back, using techniques taught in DBT could have been far more helpful, especially the distress tolerance and emotion regulation skills. Unfortunately, there is a large gap between treatment need and treatment availability when it comes to DBT. This was especially true during the pandemic. Thus, finding ways for more people to access these skills (i.e. mobile apps) is essential. In addition, DBT has show to be effectively adapted to a telehealth format. Specifically webcam-delivered comprehensive DBT has been shown to be well-received and well-attended among low-income patients.
References
Blennerhassett, R. & O’Raghallaigh, J. (2005). Dialectical behavior therapy in the treatment of borderline personality disorder. The British Journal of Psychiatry, 186(4), 278-280.
Chapman A. L. (2006). Dialectical behavior therapy: Current indications and unique elements. Psychiatry, 3(9), 62–68.
Verheul, R., van den Bosch, L., & Koeter, M. (2003). Dialectical behavior therapy for women with borderline personality disorder. British Journal of Psychiatry.182:135–40.
Colin Planalp, MPA, Giovann Alarcon, MPP, Lynn A. Blewett, PhD (May 26, 2020). 90 percent of U.S. adults report increased stress due to pandemic. The State Health Access Data Assistance Center (SHADAC). https://www.shadac.org/SHADAC_COVID19_Stress_AmeriSpeak-Survey
C. Virginia O’Hayer, Building a Life Worth Living During a Pandemic and Beyond: Adaptations of Comprehensive DBT to COVID-19, Cognitive and Behavioral Practice, Volume 28, Issue 4, 2021, Pages 588-596, ISSN 1077-7229, https://doi.org/10.1016/j.cbpra.2020.12.005.